Why the United States Leaves Deadly Chemicals on the Market
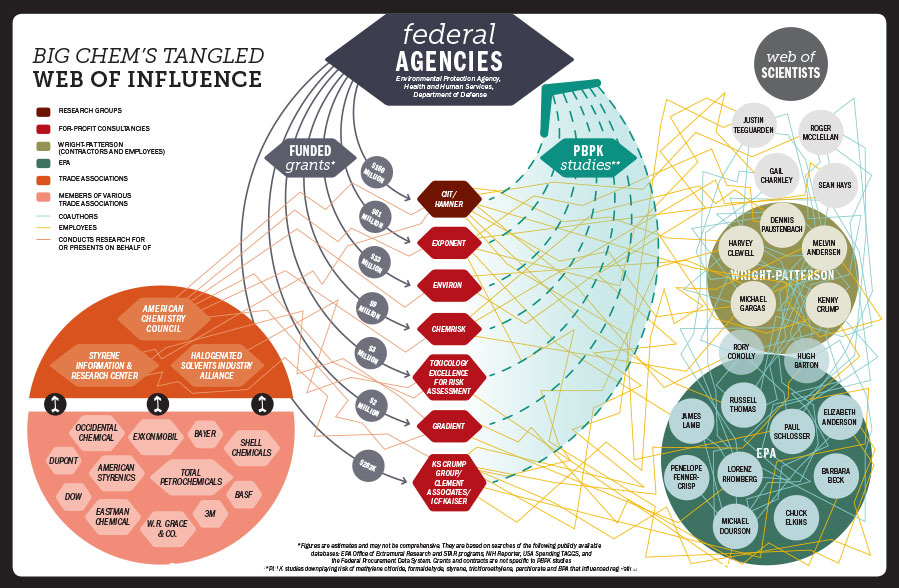
A 6-month investigation finds that the revolving door between government and the chemical industry has led the EPA to rely on easily manipulated research. The result? Toxic substances remain in everyday products.
Valerie Brown and Elizabeth Grossman

Scientists are trained to express themselves rationally. They avoid personal attacks when they disagree. But some scientific arguments become so polarized that tempers fray. There may even be shouting.
Such is the current state of affairs between two camps of scientists: health effects researchers and regulatory toxicologists. Both groups study the effects of chemical exposures in humans. Both groups have publicly used terms like “irrelevant,” “arbitrary,” “unfounded” and “contrary to all accumulated physiological understanding” to describe the other’s work. Privately, the language becomes even harsher, with phrases such as “a pseudoscience,” “a religion” and “rigged.”
The rift centers around the best way to measure the health effects of chemical exposures. The regulatory toxicologists typically rely on computer simulations called “physiologically based pharmacokinetic” (PBPK) modeling. The health effects researchers — endocrinologists, developmental biologists and epidemiologists, among others — draw their conclusions from direct observations of how chemicals actually affect living things.
The debate may sound arcane, but the outcome could directly affect your health. It will shape how government agencies regulate chemicals for decades to come: how toxic waste sites are cleaned up, how pesticides are regulated, how workers are protected from toxic exposure and what chemicals are permitted in household items. Those decisions will profoundly affect public health: the rates at which we suffer cancer, diabetes, obesity, infertility, and neurological problems like attention disorders and lowered IQ.
The link from certain chemicals to these health effects is real. In a paper published earlier this year, a group of leading endocrinologists concluded with 99 percent certainty that environmental exposure to hormone-disrupting chemicals causes health problems. They estimate that this costs the European Union healthcare system about $175 billion a year.
Closer to home, Americans are routinely sickened by toxic chemicals whose health effects have been long known. To cite one infamous example, people exposed to the known carcinogen formaldehyde in FEMA trailers after Hurricane Katrina suffered headaches, nosebleeds and difficulty breathing. Dozens of cancer cases were later reported. Then there are workplace exposures, which federal government estimates link to as many as 20,000 cancer deaths a year and hundreds of thousands of illnesses.
“We are drowning our world in untested and unsafe chemicals, and the price we are paying in terms of our reproductive health is of serious concern,” wrote the International Federation of Gynecology and Obstetrics in a statement released on October 1.
Yet chemical regulation in the United States has proceeded at a glacial pace. And corporate profit is at the heart of the story.
That the chemical industry exerts political influence is well documented. What our investigation reveals is that, 30 years ago, corporate interests began to control not just the political process but the science itself. Industry not only funds research to cast doubt on known environmental health hazards; it has also shaped an entire field of science — regulatory toxicology — to downplay the risk of toxic chemicals.
Our investigation traces this web of influence to a group of scientists working for the Department of Defense (DOD) in the 1970s and 1980s — the pioneers of PBPK modeling. It quickly became clear that this type of modeling could be manipulated to minimize the appearance of chemical risk. PBPK methodology has subsequently been advanced by at least two generations of researchers — including many from the original DOD group — who move between industry, government agencies and industry-backed research groups, often with little or no transparency.
The result is that chemicals known to be harmful to human health remain largely unregulated in the United States — often with deadly results. For chemicals whose hazards are just now being recognized, such as the common plastics ingredient bisphenol A (BPA) and other endocrine disruptors, this lack of regulation is likely to continue unless the federal chemical review process becomes more transparent and relies less heavily on PBPK modeling.
Here we lay out the players, the dueling paradigms and the high-stakes health consequences of getting it wrong.
The dawn of PBPK simulation
The 1970s and 1980s saw a blizzard of environmental regulation. The Clean Air Act, Clean Water Act and Toxic Substances Control Act, along with the laws that established Superfund and Community Right-to-Know Programs, for the first time required companies— and military bases — using and producing chemicals to account for their environmental and health impacts. This meant greater demand for chemical risk assessments as the Occupational Safety and Health Administration (OSHA) and the Environmental Protection Agency (EPA) began to establish safety standards for workplace exposures and environmental cleanups.
In the 1980s, the now-defunct Toxic Hazards Research Unit at the Wright-Patterson Air Force Base in Dayton, Ohio, was investigating the toxicity and health effects of chemicals used by the military. Of particular concern to the DOD were the many compounds used by the military to build, service and maintain aircraft, vehicles and other machinery: fuels and fuel additives, solvents, coatings and adhesives. The military is responsible for about 900 of the approximately 1,300 currently listed Superfund sites, many of which have been contaminated by these chemicals for decades.
In the mid-1980s, scientists at the Wright-Patterson Toxic Hazards Research Unit began using PBPK simulations to track how chemicals move through the body. Known as in silico (in computers) models, these are an alternative to testing chemicals in vivo (in live animals) or in vitro (in a test tube). They allow scientists to estimate what concentrations of a chemical (or its breakdown products) end up in a particular organ or type of tissue, and how long they take to exit the body. The information can then be correlated with experimental data to set exposure limits — or not.
PBPK simulations made testing faster and cheaper, something attractive to both industry and regulators. But the PBPK model has drawbacks. “It tells you nothing about effects,” says Linda Birnbaum, director of both the National Institute of Environmental Health Sciences (NIEHS) and National Toxicology Program (NTP). Observational studies and laboratory experiments, on the other hand, are designed to discover how a chemical affects biological processes.
Even regulatory toxicologists who support PBPK acknowledge its limitations: “[PBPK models] are always going to be limited by the quality of the data that go into them,” says toxicologist James Lamb, who worked for the NTP and EPA in the 1980s and is now principal scientist at the consulting firm Exponent.
The late health effects researcher Louis Guillette, a professor at the Medical University of South Carolina famous for studies on DDT’s hormonedisrupting effects in Florida alligators, put it more bluntly: “PBPK? My immediate response: Junk in, junk out. The take-home is that most of the models [are] only as good as your understanding of the complexity of the system.”
Many biologists say PBPK-based risk assessments begin with assumptions that are too narrow, and thus often fail to fully capture how a chemical exposure can affect health. For example, a series of PBPK studies and reviews by toxicologist Justin Teeguarden of the Pacific Northwest National Laboratory in Richland, Wash., and his colleagues suggested that BPA breaks down into less harmful compounds and exits the body so rapidly that it is essentially harmless. Their research began with certain assumptions: that BPA only mimics estrogen weakly, that it affects only the body’s estrogen system, and that 90 percent of BPA exposure is through digestion of food and beverages. However, health effects research has shown that BPA mimics estrogen closely, can affect the body’s androgen and thyroid hormone systems, and can enter the body via pathways like the skin and the tissues of the mouth. When PBPK models fail to include this evidence, they tend to underestimate risk.
Because of its reliance on whatever data are included, PBPK modeling can be deliberately manipulated to produce desired outcomes. Or, as University of Notre Dame biologist Kristin Shrader-Frechette, who specializes in human health risk assessment, says: “Models can offer a means of avoiding the conclusions derived from actual experiments.” In other words, PBPK models can be customized to provide results that work to industry’s advantage.
That’s not to say PBPK itself is to blame. “Let’s not throw the baby out completely with the bathwater,” says New York University associate professor of environmental medicine and health policy Leo Trasande. “However, when you have biology telling you there are basic flaws in the model, that’s a compelling reason that it’s time for a paradigm shift.”
A handy tool for industry
That PBPK studies could be used to make chemicals appear safer was as clear in the 1980s as it is now. In a 1988 paper touting the new technique, Wright-Patterson scientists explained how their modeling had prompted the EPA to stop its regulation process for a chemical of great concern to the military: methylene chloride.
Methylene chloride is widely used as a solvent and as an ingredient in making plastics, pharmaceuticals, pesticides and other industrial products. By the 1990s, the U.S. military would be the country’s second greatest user. Methylene chloride was — and remains — regulated under the Clean Air Act as a hazardous air pollutant because of its carcinogenic and neurotoxic effects.
Between 1985 and 1986, the National Institute for Occupational Safety and Health estimated that about 1 million workers a year were exposed to methylene chloride, and the EPA classified the compound as a “probable human carcinogen.” A number of unions, including United Auto Workers and United Steelworkers, also petitioned OSHA to limit on-the-job exposure to methylene chloride.
In 1986, OSHA began the process of setting occupational exposure limits. Stakeholders were invited to submit public comments.
Among the materials submitted was a PBPK study by Melvin Andersen, Harvey Clewell — both then working at Wright-Patterson — and several other scientists, including two employed by methylene chloride product manufacturer Dow Chemical. Published in 1987, this study concluded, “Conventional risk analyses greatly overestimate the risk in humans exposed to low concentrations [of methylene chloride].”
Later that year, the EPA revised its previous health assessment of methylene chloride, citing the Wright-Patterson study to conclude that the chemical was nine times less risky than previously estimated. The EPA “has halted its rulemaking on methylene chloride [based on our studies],” wrote Wright-Patterson scientists in 1988.
OSHA, too, considered the Wright-Patterson study in its methylene chloride assessment — and its rulemaking dragged on another 10 years before the agency finally limited exposure to the chemical.
The usefulness of PBPK modeling to industry did not escape the Wright-Patterson researchers. “The potential impact,” wrote Andersen, Clewell and their colleagues in 1988, “is far reaching and not limited to methylene chloride.” Using PBPK models to set exposure limits could help avoid setting “excessively conservative” — i.e., protective— limits that could lead to “unnecessary expensive controls” and place “constraints on important industrial processes.” In other words, PBPK models could be used to set less-stringent environmental and health standards, and save industry money.
So far, they’ve been proven right. The work done at Wright-Patterson set the stage for the next 30-plus years. Results obtained using PBPK modeling — especially in industry-funded research, often conducted by former Wright-Patterson scientists — have downplayed the risk and delayed the regulation of numerous widely used and commercially lucrative chemicals. These include formaldehyde, styrene, tricholorethylene, BPA and the pesticide chlorpyrifos. For many such chemicals, PBPK studies contradict what actual biological experiments conclude. Regulators often defer to the PBPK studies anyway.
A web of influence
At the time that PBPK modelling was being developed, the chemical industry was struggling with its public image. The Bhopal, India, disaster—the methyl isocyanate release that killed and injured thousands — happened in 1984. The following year, a toxic gas release at a West Virginia Union Carbide plant sent about 135 people to hospitals.
In response to these incidents, new federal regulations required companies to account for the storage, use and release of hazardous chemicals. The minutes from a May 1988 Chemical Manufacturers Association (CMA) meeting show industry was feeling the pressure. Noting the federal scrutiny and the growing testing requirements, the CMA recommended that industry help “develop exposure data” and “explore innovative ways to limit required testing to that which is needed.”
Industry had already begun to do this by founding a number of research institutes such as the Chemical Industry Institute of Toxicology (CIIT), a nonprofit toxicology research institute (renamed the Hamner Institutes in an act of linguistic detoxification in 2007). This period also saw the rise of for-profit consulting firms like Environ (1982), Gradient (1985), ChemRisk (1985) and K.S. Crump and Company (1986), with which industry would collaborate advantageously in the following decades.
“Our goal was to do the science that would help the EPA and other regulatory bodies make the policies,” explained William Greenlee, Hamner president and CEO, in an interview for a business website. Indeed, over the past 30 years, Hamner and these consultancies have produced hundreds of PBPK studies, often with the support of chemical companies or trade groups. Overwhelmingly, these studies downplay or cast doubt on chemicals’ health effects — and delay regulation.
“I have seen how scientists from the Hamner Institutes can present information in a way that carefully shapes or controls a narrative,” says Laura Vandenberg, an assistant professor of environmental health sciences at University of Massachusetts Amherst. She explains that Hamner scientists often use narrow time windows or present data in a limited context, rejecting information that does not conform to their models. “These are the kinds of tactics used to manufacture doubt,” she says.
A close look at the authors of studies produced by these industry-linked research groups reveals a web of influence traceable to Wright-Patterson (see chart on following page). At least 10 researchers employed at or contracted by Wright-Patterson in the 1980s went on to careers in toxicology at CIIT/Hamner, for-profit consulting firms or the EPA. About half have held senior positions at Hamner, including the co-authors of many of the early Wright-Patterson PBPK studies: Melvin Anderson, now a chief scientific officer at Hamner, and Harvey Clewell, now a senior investigator at Hamner and principal scientist at the consulting firm ENVIRON. “I’m probably given credit as the person who brought PBPK into toxicology and risk assessment,” Andersen told In These Times.
A revolving door between these industry-affiliated groups and federal regulators was also set in motion. More than a dozen researchers have moved from the EPA to these for-profit consultancies; a similar number have gone in the other direction, ending up at the EPA or other federal agencies.
Further blurring the public-private line, CIIT/Hamner has received millions of dollars in both industry and taxpayer money. The group stated on its website in 2007 that $18 million of its $21.5 million annual operating budget came from the “chemical and pharmaceutical industry.” Information about its corporate funders is no longer detailed there, but Hamner has previously listed as clients and supporters the American Chemistry Council (formerly the CMA, and one of the most powerful lobbyists against chemical regulation), American Petroleum Institute, BASF, Bayer CropScience, Dow, ExxonMobil, Chevron and the Formaldehyde Council. At the same time, over the past 30 years, CIIT/Hamner has received nearly $160 million in grants and contracts from the EPA, DOD and Department of Health and Human Services. In sum, since the 1980s, these federal agencies have awarded hundreds of millions of dollars to industry-affiliated research institutes like Hamner.
But the federal reliance on industry-linked researchers extends further. Since 2000, the EPA has signed a number of cooperative research agreements with the ACC and CIIT/ Hamner. All involve chemical toxicity research that includes PBPK modeling. And in 2014, Hamner outlined additional research it will be conducting for the EPA’s next generation of chemical testing — the ToxCast and Tox21 programs. Over the past five years, Hamner has received funding for this same research from the ACC and Dow.
Meanwhile, the EPA regularly contracts with for-profit consultancies to perform risk assessments, assemble peer review panels and select the scientific literature used in chemical evaluations. This gives these private organizations considerable sway in the decision-making process, often with little transparency about ties to chemical manufacturers. The upshot: Experts selected to oversee chemical regulation often overrepresent the industry perspective.
These cozy relationships have not gone unnoticed; the EPA has been called to task by both its own Office of Inspector General and by the U.S. Government Accountability Office. “These arrangements have raised concerns that ACC or its members could potentially influence, or appear to influence, the scientific results that may be used to make future regulatory decisions,” wrote the GAO in a 2005 report.
Asked for comment by In These Times, the EPA said these arrangements do not present conflicts of interest.
Decades of deadly delay
PBPK studies have stalled the regulation of numerous chemicals. In each case, narrowly focused models developed by industry-supported research concluded that risks were lower than previously estimated or were not of concern at likely exposure levels.
Take, for example, methylene chloride, the subject of the 1987 paper Wright-Patterson scientists bragged had halted the EPA’s regulatory process. Despite the chemical being identified as “probably carcinogenic to humans” by the U.N. International Agency for Research on Cancer, a “reasonably anticipated” human carcinogen by the U.S. National Toxicology Program, and an “occupational carcinogen” by OSHA, the EPA has yet to limit its use. EPA researchers noted this year that the 1987 PBPK model by the Wright-Patterson scientists remains the basis for the agency’s risk assessment.
Today, methylene chloride remains in use — to produce electronics, pesticides, plastics and synthetic fabrics, and in paint and varnish strippers. The Consumer Product Safety Commission, OSHA and NIOSH have issued health warnings, and the FDA bars methylene chloride from cosmetics— but no U.S. agency has totally banned the chemical. The EPA estimates that some 230,000 workers are exposed directly each year. According to OSHA, between 2000 and 2012, at least 14 people died in the United States of asphyxiation or heart failure after using methylene chloride-containing products to refinish bathtubs. The Center for Public Integrity reports that methylene chloride exposure prompted more than 2,700 calls to U.S. poison control centers between 2008 and 2013.
Another telling example of industry-funded PBPK studies’ influence is formaldehyde. This chemical remains largely unrestricted in the United States, despite being a well-recognized respiratory and neurological toxicant linked to nasal cancer and leukemia, as well as to allergic reactions and skin irritation. The EPA’s toxicological review of formaldehyde, begun in 1990, remains incomplete, in no small part because of delays prompted by the introduction of studies — including PBPK models conducted by CIIT/Hamner — questioning its link to leukemia.
If that link is considered weak or uncertain, that means formaldehyde — or the companies that employ the sickened workers — won’t be held responsible for the disease. The chemical industry is well aware that “more people have leukemia … than have nasal tumors,” says recently retired NIEHS toxicologist James Huff.
Some of this CIIT/Hamner research was conducted between 2000 and 2005 with funding from an $18,750,000 EPA grant. In 2010, Hamner received $5 million from Dow, a formaldehydeproduct manufacturer, for toxicity testing, including PBPK modeling. The ACC, which opposes formaldehyde restriction, also supported this research.
Consequently, apart from a few state regulations and a pending EPA proposal to limit formaldehyde emissions from composite wood products like plywood, companies can still use the chemical — as in the FEMA trailers.
Cosmetics and personal-care products can also be sources of formaldehyde exposure. This made headlines in 2011 after hair salon workers using a smoothing product called Brazilian Blowout reported nausea, sore throats, rashes, chronic sinus infections, asthma-like symptoms, bloody noses, dizziness and other neurological effects. “You can’t see it … but you feel it in your eyes and it gives you a high,” salon owner and hair stylist Cortney Tanner tells In These Times. “They don’t teach this stuff in beauty school,” she says, and no one warns stylists about these products or even suggests using a ventilator.
OSHA has issued a hazard alert for these products and the FDA has issued multiple warnings, most recently in September, but regulations prevent federal agencies from pulling the products from store shelves. So, for formaldehyde, as in the case of the paint strippers containing methylene chloride, exposures continue.
BPA rings alarm bells
The chemical currently at the center of the most heated debates about consumer exposure is BPA. The building block of polycarbonate plastics, BPA is used in countless products, including the resins that line food cans and coat the thermal receipt paper at cash registers and ATMs. While scientific evidence of adverse health effects from environmentally typical levels of BPA mounts, and many manufacturers and retailers have responded to public concern by changing their products, federal regulatory authorities still resist restricting the chemical’s use.
BPA does not produce immediate, acute effects, like those experienced by salon workers exposed to formaldehyde or machinists working with methylene chloride. But in laboratory tests on animals, BPA is a known endocrine disruptor. Structurally similar to natural hormones, endocrine disruptors can interfere with normal cellular processes and trigger abnormal biochemical responses. These can prompt numerous health problems, including cancer, infertility, and metabolic and neurological disorders. BPA has also been linked to increased risk of cardiovascular disease, diabetes and obesity.
To promote the idea that BPA is safe, the chemical industry routinely lobbies policymakers and “educates” consumers. What has not been widely discussed, however, is how industry has backed PBPK studies that marginalized research showing risks from environmentally typical levels of BPA. Many of these doubt-inducing studies have been conducted by researchers whose careers can be linked to the PBPK work done at Wright-Patterson. In published critiques, health effects researchers — among them Gail Prins and Wade Welshons — have detailed the many ways in which these PBPK models fail to accurately reflect BPA exposure.
PBPK and endocrine disruption
Over the past several decades, our evolving understanding of our bodies’ responses to chemicals has challenged previous toxicological assumptions— including those that are fed into PBPK models. This is particularly true of endocrine disruptors.
Cause-and-effect relationships between endocrine disruptors and health problems can be hard to pinpoint. We now know that early — even prenatal— exposure to endocrine disruptors can set the stage for adult disease. In addition, a pregnant woman’s exposures may affect not only her children but also her grandchildren. These transgenerational effects have been documented in animal experiments. The classic human evidence came from victims of DES, a drug prescribed in the 1940s, 1950s and 1960s to prevent miscarriages. Daughters of women who took the endocrine disruptor developed reproductive cancers, and preliminary research suggests their daughters may be at greater risk for cancer and other reproductive problems.
“The transgenerational work raises an incredible specter,” says Andrea Gore, who holds the Vacek Chair in Pharmacology at the University of Texas at Austin and edits the influential journal Endocrinology. “It’s not just what you’re exposed to now, it’s what your ancestors were exposed to.”
Complicating PBPK modeling further, hormone-mimicking chemicals, just like hormones, can have biological effects at concentrations as low as parts per trillion. In addition, environmental exposures most often occur as mixtures, rather than in isolation. And each individual may respond differently.
“PBPK doesn’t come close” to capturing the reality of endocrine disruption, the late developmental biologist Louis Guillette told In These Times, in part because modelers are “still asking questions about one chemical exposure with one route of exposure.” Even for health effects researchers, understanding of mixtures’ effects is in its infancy.
The debate over how endocrine disruption can be represented in PBPK models has intensified the unease between regulatory toxicologists and health effects researchers. That tension is particularly well-illustrated by a recent series of events that also reveal how some journal editors privilege the industry’s point of view.
A life-and-death debate
In February 2012 the World Health Organization (WHO) and the U.N. Environment Programme (UNEP) published a report intended to inform regulation worldwide. The authors were an international group of health effects researchers with long experience studying endocrine disruption.
“There is an increasing burden of disease across the globe in which [endocrine disruptors] are likely playing an important role, and future generations may also be affected,” said the report. These diseases, it continued, are being seen in humans and wildlife, and include male and female reproductive disorders, changes in the numbers of male and female babies born, thyroid and adrenal gland disorders, hormone-related cancers and neurodevelopmental diseases.
The backlash from toxicologists was immediate. Over the next few months — as the EU prepared to begin its regulatory decision-making on endocrine disruptors — the editors of 14 toxicology journals each published an identical commentary harshly criticizing the WHO/UNEP conclusions.
The commentary included a letter from more than 70 toxicologists urging the EU not to adopt the endocrinedisruption framework. The letter said that the WHO/UNEP report could not be allowed to inform policy because its science is “contrary to all accumulated physiological understanding.”
This commentary was followed by further attacks. One critique, published in the journal Critical Reviews in Toxicology, was funded and vetted by the ACC.
These commentaries infuriated health effects researchers. Twenty endocrine journal editors, 28 associate editors and 56 other scientists — including several WHO/UNEP report authors — signed a statement in Endocrinology, saying in part:
The dismissive approach to endocrine disruption science put forth … is unfounded, as it is [not] based on the fundamental principles of how the endocrine system works and how chemicals can interfere with its normal function.
Endocrinology editor Andrea Gore tells In These Times that she and other health effects researchers don’t think the scientifically demonstrated dangers of endocrine disruptors are subject to debate. “There are fundamental differences between regulatory toxicologists and what I refer to as ‘people who understand the endocrine science.’ ”
The outcome of this debate and the structure of future regulatory toxicity testing in the United States and Europe is not yet clear. The EPA appears to be attempting to incorporate endocrine disruption into PBPK models, but many scientists are skeptical the process will produce reliable results, given the models’ limitations and the complexity of endocrine effects.
From science to activism
Although couched in complex language, these arguments are not academic, but have profound implications for public health. Disorders and diseases, increasingly linked to exposure to endocrine disruptors— including metabolic, reproductive, developmental and neurological problems — are widespread and increasing. About 20 percent of U.S. adults show at least three of the five indicators of metabolic syndrome: obesity, diabetes, high blood pressure, high cholesterol and heart disease. Neurological problems, including behavioral and learning disabilities in children as well as Parkinson’s disease, are increasing rapidly. Fertility rates in both men and women are declining. Globally, the average sperm count has dropped 50 percent in the last 50 years.
Scientists typically shy away from activism, but many now believe it’s what’s needed to punch through the machinations and inertia regarding chemical regulation. Shanna Swan, Mount Sinai professor of preventive medicine, obstetrics, gynecology and reproductive medicine, notes that some of the biggest reductions in chemical exposures have happened in response to consumer pressure on both industry and policymakers. Or, as the University of California’s Bruce Blumberg says, “I think we need to take the fight to the people.”
The Endocrine Society stressed the urgency of addressing these public health impacts in a statement released September 28. Not surprisingly, industry disagreed, calling this science “unsupported” and “still-unproven.”
Meanwhile, PBPK studies continue to succeed in sowing doubt about adverse health effects of endocrine disorders. Their extremely narrow focus leads to narrow conclusions that often result in calls for more research before regulation. In regulatory decisions, “the assumption is that if we don’t know something, it won’t hurt us,” says University of Massachusetts, Amherst professor of biology R. Thomas Zoeller. In other words, the burden of proof remains on health effects researchers to prove harm, not on industry to prove safety — and proving harm is difficult, especially when other scientists are seeding doubt.
But the clock is ticking. As Washington State University geneticist Pat Hunt told In These Times, “If we wait [to make regulatory decisions] for ‘proof’ in the form of compelling human data, it may be too late for us as a species.”
This investigation was supported by the Leonard C. Goodman Institute for Investigative Reporting.






